This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Improved gene editing method could power the next generation of cell and gene therapies
A new approach to the genetic engineering of cells promises significant improvements in speed, efficiency, and reduction in cellular toxicity compared to current methods. The approach could also power the development of advanced cell therapies for cancers and other diseases, according to a study from researchers in the Perelman School of Medicine at the University of Pennsylvania.
In the study, which appeared this week in Nature Biotechnology, researchers found that protein fragments used by some viruses to help them get into cells could also be used to get CRISPR-Cas gene editing molecules into cells and their DNA-containing nuclei with extraordinarily high efficiency and low cellular toxicity.
The scientists expect the new technique to be particularly useful for modifying T cells and other cells from a patient's own body to make cell therapies. One such application could be CAR T (chimeric antigen receptor T cell) therapy, which uses specially modified immune cells from a patient to treat cancer. The T cells—a type of white blood cell—are removed from the patient and reprogrammed to find and attack cancer cells when reintroduced to the bloodstream.
The first FDA-approved CAR T therapy was developed at Penn Medicine, and received Food & Drug Administration approval in 2017. There are now six FDA-approved CAR T cell therapies in the United States. The therapies have revolutionized the treatment of certain B cell leukemias, lymphomas, and other blood cancers, putting many patients who otherwise had little hope into long-term remission.
"This new approach—building on Penn Medicine's history of cell and gene therapy innovation—has the potential to be a major enabling technology for engineered cellular therapies," said co-senior author E. John Wherry, Ph.D., Richard and Barbara Schiffrin President's Distinguished Professor and chair of Systems Pharmacology & Translational Therapeutics at Penn Medicine.
CRISPR-Cas molecules are derived from ancient bacterial antiviral defenses, and are designed to precisely remove DNA at desired locations in a cell's genome. Some CRISPR-Cas-based systems combine the deletion of old DNA with the insertion of new DNA for versatile genome editing. This approach can be used to replace faulty genes with corrected ones or delete or modify genes to enhance cellular function. Some systems can also add genes that confer new properties to CAR T cells such as the ability to recognize tumors or withstand the harsh tumor microenvironment that normally exhausts T cells.
Although CRISPR-Cas systems are already widely used as standard laboratory tools for molecular biology, their use in modifying patients' cells to make cell-based therapies has been limited—in part because CRISPR-Cas molecules can be hard to get into cells and then into cells' DNA-containing nuclei.
"Current methods of getting CRISPR-Cas systems into cells, which include the use of carrier viruses and electric pulses, are inefficient for cells taken directly from patients (called primary cells). These methods also typically kill many of the cells they are used on, and can even cause broad unwanted changes in gene activity," said co-senior author Shelley L. Berger, Ph.D., the Daniel S. Och University Professor in Cell and Developmental Biology and Genetics and director of the Penn Epigenetics Institute.
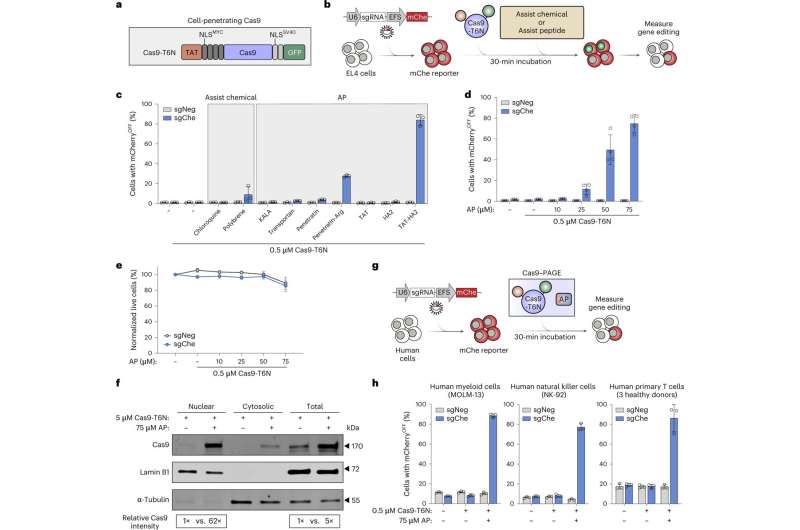
In the study, researchers explored the use of small, virus-derived protein fragments, called peptides, to pilot CRISPR-Cas molecules more efficiently through the outer membranes of primary human cells and into their nuclei. Notably, researchers found that a fused combination of two modified peptides—one found in HIV and one in influenza viruses—could be mixed with CRISPR-Cas molecules to get them into primary human or mouse cells and their nuclei with efficiencies of up to nearly 100 percent, depending on the cell type—with almost no toxicity or gene-expression changes.
The team demonstrated the approach, which they call PAGE (peptide-assisted genome editing), for several types of envisioned cell therapy including CAR T cell therapies.
In addition to its potential use in cell and gene therapies, the authors note the PAGE approach could see wide application in basic scientific research. The inefficiency of standard CRISPR-Cas cell penetration methods has meant that gene-editing to create mouse models of diseases typically requires a multi-step, time-consuming process of generating transgenic mice—to introduce the gene-editing machinery into their DNA. By contrast, PAGE with its high efficiency and low toxicity might enable rapid, efficient, and straightforward gene editing in ordinary lab mice.
"The simplicity and power of the peptide-assist concept suggests that it could potentially be adapted in the future for the delivery into primary cells of other genome-editing proteins, or even protein-based drugs," said co-senior author Junwei Shi, Ph.D., an assistant professor of Cancer Biology and member of the Penn Epigenetics Institute and Abramson Family Cancer Research Institute.
The study was a collaboration that included the laboratories of Penn co-author Rahul Kohli, MD, Ph.D., an associate professor of Infectious Diseases and Biochemistry and Biophysics, and co-author Gerd Blobel, MD, Ph.D., the Frank E. Weise III Professor of Pediatrics and co-director of the Epigenetics institute.
More information: Zhen Zhang et al, Efficient engineering of human and mouse primary cells using peptide-assisted genome editing, Nature Biotechnology (2023). DOI: 10.1038/s41587-023-01756-1
Journal information: Nature Biotechnology


















