Cancer drug could potentially be used against malaria
A cancer drug currently in clinical trials has shown the potential to protect from, cure, and prevent transmission of malaria. The breakthrough finding by an international team that includes researchers at Penn State offers new hope against a disease that kills over half a million people annually, most severely affecting children under five, pregnant women, and patients with HIV.
The research team, led by researchers at the University of Cape Town (UCT), published their results in a new paper appearing Oct. 19 in the journal Science Translational Medicine.
"Disruptions to malaria vaccinations, treatment, and care during the COVID-19 pandemic, combined with increasing reports of resistance to first-line artemisinin-based combination therapies have led to an increase of malaria cases and deaths worldwide," said Manuel Llinás, distinguished professor of biochemistry and molecular biology and of chemistry at Penn State.
"The identification of new ways to treat the disease is crucial for malaria control. Ideal treatments would operate differently than current front-line drugs to circumvent current drug resistance and act on multiple targets or stages of the parasite's life cycle in order to slow future resistance."
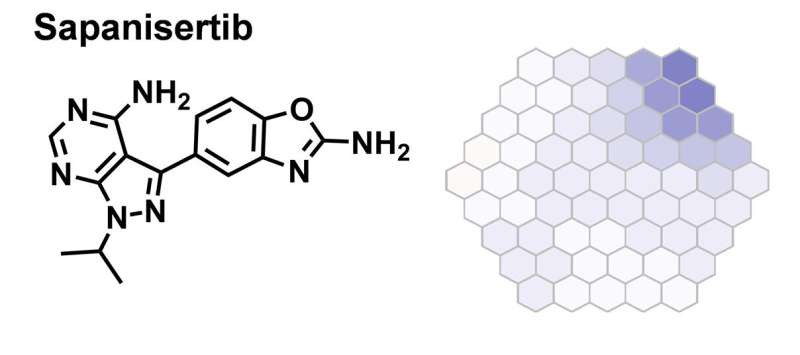
The research team explored whether sapanisertib, a drug that is currently in clinical trials for the treatment of various cancers, including breast cancer, endometrial cancer, glioblastoma, renal cell carcinoma, and thyroid cancer, could be used to treat malaria.
They found that sapanisertib has the potential to protect from, cure, and block malaria transmission by killing the malaria parasite at several stages during its life cycle inside its human host. This includes when the parasite is in the liver, where it first grows and multiplies; when it is within the host's red blood cells, where clinical symptoms are observed; and when it divides sexually within the host red blood cells to produce the transmissible forms of the parasite. The transmissible form is typically taken up by the female Anopheles mosquito during a blood meal and passed on during subsequent blood meals to infect another person, so killing the parasite should also prevent subsequent infections.
The researchers also established the mechanism by which sapanisertib kills the human malaria parasite and found that the drug inhibits multiple proteins called kinases in the malaria parasite.
Sapanisertib's multistage activity and its antimalarial efficacy, coupled with potent inhibition of multiple protein targets—including at least two that have already been shown to be vulnerable targets for chemotherapeutic intervention—will underpin further research to evaluate the potential of repurposing sapanisertib to treat malaria.
Repurposing existing drugs
The research team took advantage of an approach known as drug repurposing, which aims to find new uses for an existing drug, approved by a regulatory agency in one disease area, for another disease. This approach is used to circumvent challenges with discovering and developing a new medicine from scratch, which is a lengthy and expensive process, often with low returns in terms of the number of drugs that finally make it to the market.
"The problem is amplified in neglected and tropical diseases such as malaria where existing resources are strained and the financial returns low," said Kelly Chibale, founder and director of the UCT Drug Discovery and Development Centre, Neville Isdell Chair in African-centric Drug Discovery and Development at UCT, and leader of the research team. "The drug repurposing approach of investigating existing drugs as potential therapies for other diseases shortens the process as in most cases the candidates, in this case sapanisertib, will have been through several stages of clinical development and will have well-known exposure and safety profiles in humans."
While new uses for approved drugs have sometimes been found serendipitously in the drug repurposing approach, strategies exist to rationally identify drugs that can be used for other diseases. In this study, the team exploited drugs that act through protein targets of human origin, which might be active in similar protein targets in the malaria parasite.
Working as part of the Malaria Drug Accelerator project, Tarrick Qahash, an undergraduate turned technician in the Llinás lab at Penn State, used mass spectrometry-based metabolomics to determine the parasite's response to a variety of antimalarial drugs.
"In cancer, sapanisertib inhibits a protein kinase called mTOR that regulates a variety of cellular processes, including immune response and autophagy. However, until this study, it was unclear how it would affect the malaria parasite," said Llinás.
"We used a process called metabolic fingerprint profiling and found that the parasite's response to sapanisertib resembled inhibition by other protein kinase inhibitors we had investigated. Through its effects on the parasite's metabolism of hemoglobin—a protein that carries oxygen through the blood—we determined that sapanisertib primarily inhibits the kinase called PfPI4Kβ, but we also found that it can target a kinase called PKG."
Kinases have been extensively investigated as therapeutic targets in many diseases because of their importance in cellular function. This makes them attractive for repurposing in other diseases, including malaria. Kinase targets essential to multiple stages of the malaria parasite life cycle have in fact already been identified.
Potential impact
This study opens new avenues for the rational development of malaria drugs designed to inhibit two or more protein targets in the malaria parasite. This could also have advantages for patients in a clinical setting, as it is more challenging for the parasite to develop resistance to a drug that kills through multiple mechanisms.
Recognizing the potential safety concerns of using a cancer drug in treating malaria, the research team is now working to understand the drivers of sapanisertib efficacy, the corresponding dose requirements, and therapeutic window for malaria. The aim is to compare how sapanisertib's predicted human dose for malaria differs from the maximum tolerated dose that is used to treat cancer.
"This work highlights the importance of local and international research partnerships to solve critical human challenges based on mutual interest and responsibility," said Chibale. "It demonstrates how advances in science and medicine can be made when industry and academic institutions share knowledge and expertise."
More information: Lauren B. Arendse et al, The anticancer human mTOR inhibitor sapanisertib potently inhibits multiple Plasmodium kinases and life cycle stages, Science Translational Medicine (2022). DOI: 10.1126/scitranslmed.abo7219
Journal information: Science Translational Medicine
Provided by Pennsylvania State University





















